People with functional gastrointestinal (GI) disorders can have a variety of symptoms that range from painless diarrhea or constipation to pain associated with diarrhea and/or constipation (usually called irritable bowel syndrome). There is another, less common condition of abdominal pain that is chronic or frequently recurring; it is not associated with changes in bowel pattern or with another medical condition. This condition is called centrally mediated abdominal pain syndrome (CAPS) – formerly known as functional abdominal pain syndrome (FAPS).
CAPS is a functional GI disorder. There are no abnormal x-rays or laboratory findings to explain the pain. It occurs because of altered sensitivity to nerve impulses in the gut and brain, and it is not associated with altered motility in the intestines. CAPS is characterized by continuous or frequent abdominal pain that is often severe. It has little or no relationship to events such as eating, defecation, or menses.
For people with CAPS, the pain can be so all-consuming that it becomes the main focus of their life. Not only does it impact quality of life, but it has a major economic impact as well.
Pathophysiology – Understanding Why People Get CAPS
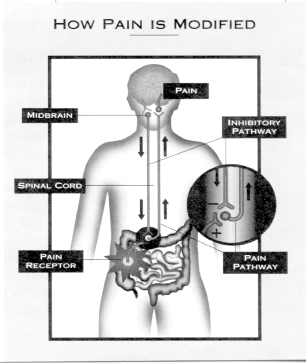
To understand the basis for Centrally mediated abdominal pain syndrome it is helpful to understand how the body experiences pain. Nerve impulses travel from the abdomen to the spinal cord, and then to various areas of the brain.
There are many different areas of the brain involved in the sensation of abdominal pain. One of these connected areas is concerned with the location and intensity of the pain, while another connected area is concerned with memories or emotions. Because of this interconnection, the perception of pain can be affected by emotions or life experiences.
While symptoms of CAPS can appear without apparent cause, they can also occur after infections or events that stimulate the bowel and also after traumatic life events like the death of a loved one, a divorce, or a history of abuse. During times of added stress, symptoms can worsen.
Repeated injury in the abdomen can cause nerve receptors to become overly sensitive. For instance, if someone has had multiple abdominal surgeries or an infection, a later painful occurrence may be experienced as more painful than previously.
Even normal abdominal activity may be experienced as being painful. It is as if the volume has been turned up on a stereo receiver. This condition is called visceral hypersensitivity (increased sensitivity of the intestines).
Furthermore although the brain has an ability to “turn down” the pain signals from the GI tract with CAPS, this ability is reduced, so even small amounts of intestinal disturbance can be amplified to produce severe pain (central hypersensitivity). So these individuals have an altered “brain-gut axis” where there is a failure of the brain to regulate even normal gut nerve activity leading to increased pain.
Understanding how the brain can modify the pain experience (for better or worse) is essential to beginning any treatment. When someone is feeling anxious or depressed, or focuses attention on the pain, it is experienced as more severe. The use of relaxation training or other techniques can divert attention away from the pain.
If a person has previously had a bad encounter with pain, the fear of having the pain again can actually make the pain worse the next time. If a person takes steps to feel in control of the pain, symptoms will improve. In addition, the amount of support a person receives from family, friends, and other sources can affect how a person responds to pain.
Treatment Strategies for Functional Abdominal Pain Syndrome
Given what we currently know about CAPS, the aim of treatment is to help you gain control over your symptoms and improve daily function, rather than totally eliminate symptoms, which usually is not possible.
One way to start is to keep a diary to record symptom flare-ups, and to identify possible triggers (emotional and situational). This kind of information may be used by you or your physician to help develop better strategies to control the symptoms.
The brain not only affects how you sense pain, it is also able to block pain. Think about the basketball player who sprains his ankle during a game and continues to play without awareness of pain. Then, when the game ends, he collapses to the floor, unable to walk. He was able to block the pain by focusing his attention on the game.
When nerve impulses travel up from the abdomen to the spinal cord, some of them go through a kind of “gate” that is controlled by nerve impulses coming down from the brain. These impulses from the brain can block or inhibit pain signals going from the abdomen to the brain by “closing” the gate. Alternatively, they can increase signals to the brain by opening the gate.
Because the brain has such a strong influence on the sensation of pain, psychological treatments can relieve symptoms of CAPS by sending signals that close the gate. Different techniques include relaxation, imagery, hypnosis, and cognitive-behavioral therapy.
Treatments – The Mind-Body Connection
- Symptom diaries – Help you see what events or emotions make symptoms worse.
- Stress management (i.e., relaxation techniques, meditation) – Teaches you how to focus attention on something other than the pain.
- Hypnosis – Helps you focus attention away from the pain. Positive suggestion can change ways you think or react.
- Cognitive-behavioral therapy – Teaches you how to change non-helpful thoughts, perceptions, and behaviors to control symptoms.
Medications may also be used in the treatment of CAPS. For continuous or severe abdominal pain, your doctor might prescribe an antidepressant. It is important to understand that these medications are not just used to treat individuals who have depression but also act as pain relievers (central analgesics) for treatment of CAPS and many other painful conditions.
Antidepressant medications can help stimulate the brain to increase the signals which block pain transmission from the abdomen to the brain. It may take several weeks before a difference is noticed.
Treatments – Antidepressant Medications
- Antidepressants act as pain relievers.
- These medications stimulate the brain to send signals and close the pain-control gate in the abdomen.
- Antidepressants might take several weeks to work, so you shouldn’t stop taking them until your doctor tells you to do so.
- Side effects are possible but usually go away after a few days.
Some people will experience side effects from antidepressant medications. Usually, the side effects will go away after a few days so it is important to stay with the medication until treatment benefit is obtained.
The tricyclic antidepressants (TCAs) can cause dry mouth and drowsiness. Another group of antidepressants is called selective serotonin norepinephrine reuptake inhibitors (SNRIs). These can cause side effects like nausea. Both of these classes of antidepressants are helpful for treating pain.
Finally, it is becoming increasingly common to use combinations of treatments like a medication for the bowel and an antidepressant or two types of medications to affect the brain’s pain control or a behavioral treatment like cognitive behavioral treatment with an antidepressant. These combinations can improve the pain benefit while keeping side effects at a minimum.
The Patient-Doctor Partnership
It is important that you work with a physician who demonstrates empathy toward you and an understanding of the symptoms of CAPS. It is a disorder where treatment requires the participation of both you and your physician.
Treatments for CAPS are most effective when the patient and the doctor work as a team, each having a role. Your doctor has the responsibility to educate you about CAPS. He or she should answer your questions and provide you with an understanding of what your symptoms are about and what your treatment options are.
You need to express your views about your treatment goals, work with your doctor to develop the treatment plan, and work toward putting the plan into action. If you follow the treatment plan closely, you and your doctor will be better able to track your results. This will allow you to achieve the best possible relief of abdominal pain.
Source
Adapted from Chronic Functional Abdominal Pain Syndrome IFFGD Publication #141 by Douglas A. Drossman, MD, Drossman Gastroenterology, Drossman Center for the Education and Practice of Biopsychosocial Care, Chapel Hill, NC.
