Note: Many disorders can affect the digestive tract. Some can have symptoms that may be similar to or overlap with gastrointestinal (GI) functional or motility disorders. These will have uniquely identifying features which differentiate them from functional GI or motility disorders.
What is Diverticulosis and Diverticulitis?
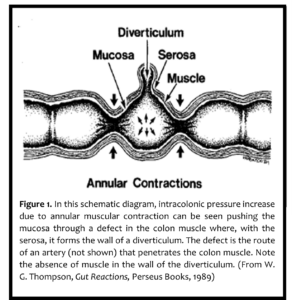
Diverticulum: (singular) is an outpouching of the wall of the gut to form a sac or pouch.
Diverticula: (plural) may occur at any level from the esophagus to the colon.
Diverticulosis: The condition of having a diverticulum or diverticula is called” diverticulosis
Diverticulitis: Inflammation of a diverticulum and the surrounding tissue is called diverticulitis.
Read more about the difference between Diverticula, Diverticulosis, and Diverticulitis
Types of Diverticulitis
Diverticulitis is divided into “uncomplicated” and “complicated” diseases.
Complicated diverticulitis is when there are complications or recurrent symptoms. Complicated diverticulitis is often diagnosed when a pocket of pus (also known as abscess) is found in the colon or when a hole (or perforation) in the small intestine or colon occurs.
Patients with a pelvic or abdominal abscess can become very ill, and the abscess fluid (pus) must be drained through a large needle directed by a radiologist, or a surgeon. In very severe cases, the colon above the abscess is brought out to the skin by a surgeon and the intestinal contents are temporarily collected in a bag. This is called a colostomy. Later, when the infection has settled down, the affected
colon is removed, and the colon rejoined.
In some rare cases, peritonitis can occur. Peritonitis is life-threatening and requires emergency surgery. It is when there is a perforation of the peritoneum (the area between your skin and most of your visceral organs including the lungs, the heart, and the organs of the digestive, excretory, reproductive, and circulatory systems.) causing peritonitis.
Complications of severe diverticulitis can cause narrowing of the colon which can lead to obstructions or fistulas (abnormal connections between body parts which in this case can include the colon to the bladder, small bowel, vagina, or other parts of skin). These complications are rare and should not concern those who have uncomplicated diverticula.
Uncomplicated diverticulitis is more common than complicated diverticulitis. It is diagnosed when the diverticula are found with episodes of localized abdominal pain associated with infection and inflammation.
Symptoms
There is controversy about whether diverticula can cause symptoms by themselves, without overt inflammation present. Some healthcare providers would treat symptoms of abdominal pain, bloating, and changes in bowel movements (diarrhea or constipation) as diverticular disease, while other healthcare providers would treat these symptoms as irritable bowel syndrome (IBS). Diverticulosis and IBS are very common, so you can have both at the same time, although one may not cause the other.
It is important to give your healthcare provider a description of how frequently you get belly pain, what it feels like, what triggers it, and if other factors are present, like fever, vomiting, or diarrhea.
Diverticular Bleeding
Arteries often run within diverticula. Though uncommon, these same arteries can gradually wear through the thin wall of the diverticulum and cause bleeding that is sometimes life-threatening. The earliest symptoms are faintness and the appearance of very bright red blood in the rectum. Such a complication requires hospitalization and blood transfusion.
A special kind of CT scan (CT angiogram or bleeding scan) can be performed to locate the source of bleeding. Radiologists may also perform a procedure called an angiography (a type of x-ray used to check blood cells) to try to locate the source of bleeding in real time and treat it. A Colonoscopy is sometimes attempted but can be technically difficult with active bleeding.
Fortunately, the bleeding usually stops on its own, but can recur in about one-quarter of cases. In rare cases, a surgeon must operate to remove the segment of the colon containing the bleeding diverticulum.
Prevention
The best way to help prevent diverticulitis is to keep diverticulosis under control. That means eating a high fiber diet – which requires 20 to 35 grams of fiber each day. Fiber is found in grains, vegetables, and fruits. Also, it is important to drink enough fluids – at least eight glasses – throughout the day to help keep stool soft.
Learn more about nuts, seeds, and diverticula
Treatment
Treatment of “uncomplicated” diverticulitis usually consists of a low-residue/low-fiber diet and rest until symptoms improve. Studies show that people get better at the same rate whether they get antibiotics or not. However, those living with compromised immunity or who experience repeated or complicated episodes of diverticulitis may benefit from antibiotics.
Adapted from “Diverticula, Diverticulosis, Diverticulitis: What’s the Difference?” By: Joy Liu, MD, Northwestern University- Feinberg School of Medicine, Chicago, IL. Adapted from article by W. Grant Thompson, M.D., F.R.C.P.C., F.A.C.G., Professor Emeritus, Faculty of Medicine, University of Ottawa, Ontario, Canada.














