Inflammation can be a normal response to injury, or an abnormal response that causes disease. Inflammation can cause symptoms like fever, pain, swelling, and discomfort. Non-steroidal anti-inflammatory drugs (NSAIDs) treat inflammation by decreasing the activity of a group of enzymes called cyclooxygenases (COX). NSAIDs are often recommended after dental procedures and surgeries. They are commonly used to treat inflammatory conditions, headaches, sore muscles, arthritis, period pain, and other aches and pains.
Be sure to discuss the use of any drug with your doctor so that you understand how to use it as directed, are familiar with the risks as well as benefits, and know what to do if side effects occur or symptoms return.
What are NSAIDs
NSAIDs is an acronym for “non-steroidal anti-inflammatory drugs.” The steroids referred to here are not those employed by wayward athletes, but rather those of the adrenalcortical steroid family such as hydrocortisone, prednisone, and betamethasone.
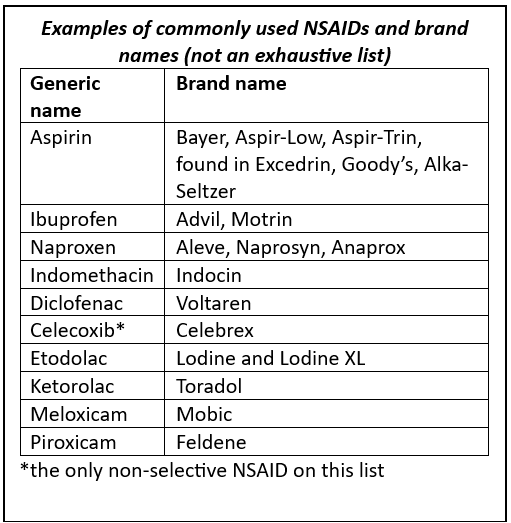
Because they suppress inflammation they are employed in many chronic inflammatory diseases such as rheumatoid arthritis. Unfortunately, these drugs have important metabolic effects that limit their use. NSAIDs are a class of drugs that suppress inflammation through inhibition of the enzyme cyclooxygenase (COX). They have important analgesic (pain killing) effects as well. Examples are listed in Table 1.
Ulcers and other intestinal problems
Turning off the COX enzyme (specifically, COX-1) has the unintended side effect of decreasing prostaglandins in the stomach. Prostaglandins in the stomach maintain the mucus and bicarbonate layer that protects the lining from stomach acid. Without prostaglandins, it becomes easier for stomach acid to damage the stomach and nearby small intestine. Through other mechanisms, NSAIDs are associated with damage to other parts of the small intestine and colon. Besides ulcers, NSAIDs can be associated with:
- “Erosions”=mild irritation of the intestines
- “Ulcers”=damage that causes penetration through the top part of the intestinal lining
- “Gastritis”=stomach inflammation
- “Enteritis”=small intestine inflammation
- “Colitis”=colon inflammation
- Rarely, “Strictures”=intestinal narrowing that can lead to blockages
Some NSAIDs have a higher risk of causing intestinal damage than others. For example, naproxen and indomethacin are statistically more likely to be associated with ulcers than ibuprofen. Just because an NSAID is labeled “enteric-coated” does not mean it is a guarantee against ulcer formation.
How NSAIDs Work
NSAIDs decrease the activity of COX enzymes. COX-1 is an enzyme that maintains “housekeeping” function in the body, including making blood flow higher or lower, blood clotting, and intestinal barrier protection against stomach acid. COX-2 is an enzyme that is involved in processes associated with inflammation, pain, and wound healing. NSAIDs can be “selective” (decreasing COX-1 activity) or “non-selective” (decreasing COX-1 and COX-2 activity). While selective NSAIDs are associated with a lower risk of GI side effects, they have been associated with a higher risk of cardiovascular side effects. In fact, two selective NSAIDs (Vioxx and Bextra) were taken off the market for this reason.
NSAIDs cause the most amount of damage in the first 30 days of use. NSAID intestine injury and ulcers are most likely in people who are taking large doses over a relatively short period of time, such as after surgery, or for a muscle sprain. NSAIDs come in a variety of forms: tablets, liquids, creams, gels, and injections. Sometimes they are combined with other medications, including cold medications and pain killers, so always be sure to check the label to see if you could be using an NSAID. All forms of NSAIDs have the potential to cause GI side effects but creams and gels have a more limited effect.
What about aspirin?
Aspirin is an NSAID. It has a strong proven benefit for heart health, and a relatively low likelihood of causing intestinal damage, so its benefits should be weighed against the risks. In most people, it will be more beneficial to use aspirin than to not use aspirin. A lower dose is considered less likely to cause side effects than a higher dose (i.e., 81 milligrams of aspirin is safer to take than 325 milligrams) but may also not be as strong. If you are not taking aspirin for any specific reason (like preventing a second heart attack, history of stroke, a family history of heart disease, etc.) it is worth considering whether you should take aspirin at all.
Are there alternatives to NSAIDs I can take for common aches and pains?
Talk to your healthcare provider about what doses and how often you can use alternatives below:
- Acetaminophen (Tylenol) is a recommended alternative for reducing fever and pain relief. It is not an NSAID.
- NSAID creams do not have the same risk of causing ulcers as oral NSAIDs.
- Heat and gentle stretching and exercise, including a physical therapy program.
Chronic pain, lasting more than 6 months, or new severe pain should always be discussed with a healthcare provider, as these kinds of pains may require a treatment plan or may be a sign of an underlying condition.
When should NSAIDs be avoided?
If you have a history of ulcers associated with bleeding, bowel blockage, or that required surgery, it is likely that the risk of harm from NSAIDs outweighs the benefits. You should seek recommendations from your healthcare provider. If NSAIDs are required, often people may take an acid blocker like proton pump inhibitors (PPIs) to reduce the risk of ulcers.
**Generally, people with inflammatory bowel disease (IBD) are recommended to avoid NSAIDs.
If you are already chronically using steroids, or above the age of 75 years, NSAIDs may be more likely to cause side effects. NSAIDs can also have cardiovascular and kidney side effects, so you should also talk with your healthcare provider if you have a history of chronic kidney disease, serious cardiovascular disease, bleeding disorders, take blood thinners, and review your medication list with your team.
On July 9, 2015, The U.S. Food and Drug Administration (FDA) announced strengthening an existing label warning that non-aspirin nonsteroidal anti-inflammatory drugs (NSAIDs) increase the chance of a heart attack or stroke. Learn more here.
On July 18, 2005 the FDA issued supplemental request letters to sponsors of all non-steroidal anti-inflammatory drugs (NSAIDs) requesting that they make labeling changes to their products. These letters included recommended proposed labeling for both the prescription and over-the-counter (OTC) NSAIDs and a medication guide for the entire class of prescription products.
All sponsors of marketed prescription non-steroidal anti-inflammatory drugs (NSAIDs), including Celebrex (celecoxib), a COX-2 selective NSAID, were being asked to revise the labeling (package insert) for their products to include a boxed warning, highlighting the potential for increased risk of cardiovascular (CV) events and the well described, serious, potential life-threatening gastrointestinal (GI) bleeding associated with their use. The Celebrex labeling will, in addition to the general labeling that will apply to all NSAIDs, also contain safety data from long-term treatment trials with celecoxib.
Manufacturers of non-prescription (over-the-counter) NSAIDs were being asked to revise their labeling to provide more specific information about the potential CV and GI risks of their individual products and remind patients of the limited dose and duration of treatment of these products in accordance with the package instructions.
On April 7, 2005 the FDA asked Pfizer to voluntarily remove Bextra (valdecoxib) from the market.
On September 30, 2004 Merck & Co., Inc. announced a voluntary withdrawal of Vioxx (rofecoxib) from the U.S. and worldwide market due to safety concerns of an increased risk of cardiovascular events (including heart attack and stroke) in patients on Vioxx.
Adapted from “Non-steroidal anti-inflammatory drugs (NSAIDs) and Ulcer Disease“- IFFGD Publication #519 by Joy J. Liu, MD, Instructor, Feinberg School of Medicine, Northwestern Medicine
** Beginning September 2019, the US Food & Drug Administration (FDA) is alerting health care professionals and patients of specific recalls of ranitidine (Zantac). Find FDA details here