The human gut microbiome is a living and dynamic ecosystem within the digestive tract that consists of trillions of microorganisms including bacteria, archaea, fungi, viruses, and protozoans.
The four dominant groups that make up most of the human gut microbiome are:
- Bacteroidetes
- Firmicutes
- Actinobacteria
- Proteobacteria
The composition of the gut microbiome varies throughout the digestive tract, with the stomach and small intestines containing fewer bacteria than the colon (large bowel).
There are more bacterial cells in our digestive tract than human cells in our body!
Everyone’s digestive system has a unique collection of microorganisms. The number and composition of microbes in our bowels can vary depending on many things like how we were born, diet, medications, genetics, where we live and what we are exposed to in our environment. Even two healthy people can have very different microbiomes.
What are the functions of the gut microbiome in humans?
The gut microbiome plays an important part in keeping us healthy and making sure that our body works properly.
First, it helps us digest food and breaks down complex carbohydrates like starches and fibers. Fermentation of indigestible fibers creates short chain fatty acids (SCFAs), such as acetate, propionate, and butyrate, which can be used by the body as a nutrient source. SCFAs also further strengthen the lining of our guts.
Select gut microbes have an essential role in production of vitamins such as vitamin B and K, biotin, thiamine, cobalamin, riboflavin, and pantothenic acids.
The gut microbiome also helps regulate our immune system. The digestive tract lining acts as a protective barrier against pathogenic microbes. When a balanced group of microbes reside in the gut, they compete with pathogenic organisms and prevent an overpopulation of potentially harmful microbes. Gut microbes also secrete compounds that stop the growth of pathogens. Certain microbes can create molecules such as gamma amino butyric acid (GABA), which can affect the function of our brain. The gut microbiome also helps by modifying insulin resistance and blood sugar balance, breaking down harmful food compounds and helping with medication metabolism
What factors can shape the composition of the gut microbiome?
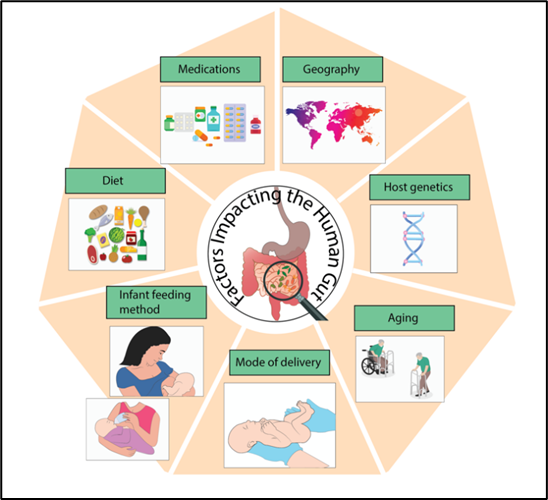
The gut microbiota in healthy adults tends to remain stable over time, but there are many factors that help shape the composition of the gut ecosystem. These factors include method of infant delivery, diet, aging, host genetics, medications, where we live and other environmental exposures.
Healthy gut microbiomes can be very different, making it hard to determine what is considered abnormal. However, healthy microbiomes usually include high microbial diversity, healthy levels of short chain fatty acids, an intact gut lining (mucosal barrier) and the absence of inflammation.
The gut microbiome was thought to form when we are born, but newer data has shown that microbes are first present in utero. Microbes have been found in the placenta, amniotic fluid and umbilical cord.
When the baby is born, they are exposed to a wide range of microorganisms. An infant born of vaginal birth receives a wide range of bacteria from the vagina of the birth mother (vaginal flora). This leads to larger populations of Bacteroides than Firmicutes compared to those born of cesarean section. Infants born by cesarean delivery receive skin flora (communities of microorganisms that reside on the skin). The human gut microbiome is also influenced by whether the baby is breastfed or formula fed. As the baby grows, the gut microbiome continues to evolve, and diet continues to shape the composition of the microbiome.
Aging also affects the gut microbiome and elderly people have decreased microbial diversity, increased abundance of opportunistic pathogens and decreased short chain fatty acid producing species.
Host genetics also affect the gut microbiome and the likelihood of a person’s susceptibility to pathogens. Some bacteria in the gut can run in families. In fact, identical twins that have lived far apart for years and family members can have similar gut microbial profiles whereas marital partners who live together and eat similar foods do not.
Location also affects the composition of the human gut microbiome. This is most likely due to variations in the climate, genetics, and dietary factors.
Medications can also impact the gut microbiome. Antibiotics can be seen as both good and bad. They can kill both beneficial and harmful gut microbes. Most often the gut microbiome recovers after antibiotic therapy but sometimes the balance of gut microbes is disturbed, and this impacts the ability of healthy microorganisms to compete with harmful pathogens to occupy the intestinal lining.
What happens when there is a disturbance?
The human gut microbiome has microbes that are both helpful and potentially harmful for humans, however the majority of gut microbes are non-pathogenic and have a symbiotic relationship with humans, meaning both the human body and gut microbes’ benefit. A smaller number of microbes are pathogenic, meaning they can promote various diseases.
When there is a disturbance to the gut microbiome, there is reduced microbial diversity, increased levels of pathogens, disruption of the gut mucosal barrier and inflammation. This can make the body more susceptible to various diseases.
Alterations in the gut microbiome have been seen in many diseases including obesity, diabetes, small intestinal bacterial overgrowth, irritable bowel syndrome, inflammatory bowel disease, allergic disease, autoimmune diseases, neurodevelopmental illnesses, and colon cancer.
Conclusion
Our digestive tract contains trillions of microorganisms that make up our unique gut microbiome. This ecosystem of microorganisms plays significant roles for human health including digestion, metabolism, vitamin synthesis, immunity, and neuropsychiatric function. The microbiome evolves over a person’s lifetime and is affected by type of birth, diet, medications, genetics, age, and other environmental exposures. When dysbiosis or an imbalance to the microbiome occurs, the body can become more susceptible to diseases that can impact the gastrointestinal, metabolic, immunological, and neurologic systems.
Taken from IFFGD fact sheet 279: The Human Gut Microbiome Jane Lim, M.D., M.S Motility Fellow and Edited by Ali Rezaie, M.D., M.Sc, Associate Professor, GI Motility Program, Karsh Division of Gastroenterology and Hepatology, Cedars-Sinai Medical Center, Los Angeles, California
This Fact Sheet is being provided in part by bioMérieux and Seres Therapeutics and donors of IFFGD.














