What is bloating and distension?
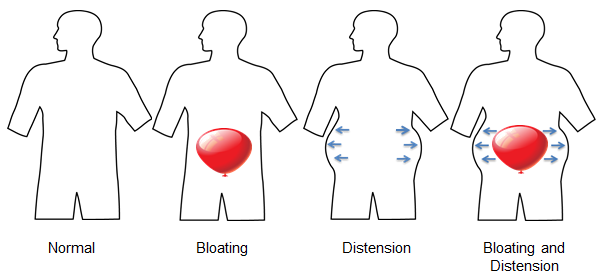
Bloating can be described as the feeling that there is an inflated balloon in the abdomen. It is a commonly reported symptom and is sometimes associated with distension, or the visible increase in the width of the area between your hips and chest (abdominal girth).
Both bloating and distension cause discomfort, and sometimes pain, and have a negative impact on the quality of life for some individuals. The symptoms may be linked with other gas related complaints, such as burping or belching (eructation), swallowing air (aerophagia), and passing intestinal gas (flatulence).
Learn more about controlling intestinal gas
– IBS: 23%-96%
– Functional dyspepsia: 50%
– Chronic constipation: 56%
Some people with functional gastrointestinal disorders (FGIDs) and motility disorders frequently experience bloating, distension, or both as symptoms of their conditions. There is also something called functional bloating, which is fullness and or/distension of the abdomen, not associated with changes in bowel movements.
Causes
While researchers have proposed several different explanations for bloating and distension, there is no conclusive answer as to why the two symptoms occur.
Possible reasons for bloating and distension include:
- Too much gas in the intestine
- Abnormal levels of bacteria in the small intestine (small intestinal bacterial overgrowth – SIBO)
- Imbalance of microorganisms that usually live in the bowel (dysbacteriosis); sometimes the result of taking antibiotics
- Food intolerance
- Increased perception and sensitivity to what is happening in the digestive tract
- Increased curvature of the lumbar region of the spine (lumbar lordosis), which decreases the capacity of the abdomen to hold gas
Bloating and Gastroparesis
Gastroparesis is a motility disorder in which the muscle contractions that move food along the digestive tract do not work properly and the stomach empties too slowly.
Reports from highly specialized (tertiary) medical centers that often see people with severe gastroparesis suggest that bloating is a common symptom. Bloating severity appears to be related to the intensity of other gastroparesis symptoms, but is not affected by gastric emptying rates. Antiemetics, probiotics, and antidepressants with significant norepinephrine reuptake inhibitor activity may help.
The main symptom of bacterial overgrowth (SIBO), a condition that sometimes accompanies gastroparesis, is bloating. Careful use of antibiotics and probiotics may be helpful in the management of these symptoms.
Treatment
There is no universally effective treatment for bloating and distension. Treatment availabilities vary from country to country and there are many underlying possibilities as to what is causing the symptoms. However, despite the fact that there isn’t an easy answer for bloating or distension, there are things that people can do with the help of their physicians to try and alleviate the symptoms.
Working with a healthcare provider
It is important to speak openly and honestly with your physician to express a clear picture of your experiences and symptoms. FGIDs present special challenges when communicating, specifically because of their vague symptoms and sensitive subject matter.
There isn’t a diagnostic test for bloating or distension; however, your healthcare provider may run some tests to rule out underlying problems or associated disorders.
For more information about GI tests and how to prepare for them, see our website www.aboutGIMotility.org or see IFFGD publications #111 or #510.

These tests include:
- Stool analysis
- Blood workup
- Abdominal x-rays
- Barium swallow
- Small transit follow through
- Barium enema
- Gastric emptying tests
- Esophageal, antroduodenal, or anorectal manometry
- Colonic transit studies
- Breath test
- Upper endoscopy
- Colonoscopy with biopsies
Learn how to prepare for tests
Individuals can help their physicians by describing their complaints as accurately and concisely as possible. With regard to bloating and distension, here are some important questions to ask and details to tell your health care provider (keeping track of the things that trigger your symptoms is a good way to discover the answers):
Things to Ask Your Healthcare Provider:
- Am I bloated?
- Am I distended?
- Am I both bloated and distended?
Things to Tell Your Healthcare Provider:
- Is the symptom located in the upper or lower abdomen?
Is it in a concentrated area? - Is your bloating or distension associated with burping?
- Do you experience nausea or vomiting?
- Is the symptom associated with pain in your abdomen?
Upper or lower? - Does the bloating or distension relate to passing gas or a change in your bowel habits (diarrhea, constipation, or alternation of both)?
- Are your symptoms related to food? Which ones?
- Do they occur right after eating?
- Do your symptoms increase during the day or improve during night hours?
Medications and other therapies
Some medications and other treatments have been found to help ease the symptoms of bloating and distension. Your doctor may talk to you about some of these options, depending on your symptoms and other health related considerations.
Antispasmodics: These can relax the muscles of the bowel and provide relief. Examples include dicyclomine (Bentyl) and hyoscyamine (Levsin) in the United States and otilonium bromide or pinaverium bromide available in Latin America and some countries in Europe and Asia and a combination of pinaverium bromide with simethicone (Alevian Duo) in some Latin America countries.
Learn more about antispasmodics
Probiotics: These dietary supplements contain live bacteria that help balance out the existing bacteria of the intestines. Some that include a relatively low level of probiotic bacteria are available over the counter or in yogurt varieties. Other options include Bifidobacterium infantis 35624 for individuals with irritable bowel syndrome (IBS) in general, and Bifidobacterium animalis DN-0173 10 for patients with IBS with constipation (IBS-C).
Rifaximin: This antibiotic is only slightly absorbed and can be used for short periods of time. Usually it is used (off-label) to lessen bloating in people with IBS whose symptoms do not include constipation, or in those with small intestinal bacterial overgrowth.
Prokinetics: These are medications that improve the time it takes for food to travel through the digestive tract. Some prokinetics have been shown to improve bloating. A person’s age, health and other considerations must be taken into account for these therapies and availabilities vary from country to country.
Learn more about prokinetics (also called promotility agents)
Antidepressants: These drugs affect receptors in the gut and in the brain. Given in lower dosages than what is used to treat depression, they have been shown to help alleviate bloating and distension. For example, citalopram (Celexa), an SSRI (selective serotonin reuptake inhibitor), has been shown to help improve bloating in individuals with IBS. Amitryptiline (Elavil), a tricyclic antidepressant, is commonly used to treat pain and discomfort, as well as diarrhea, and may be helpful for bloating.
Other options: Medications that increase fluid content in stools, lubiprostone (Amitiza) or linaclotide (Linzess) for example, may also be used.
Psychological therapies: Treatments including hypnotherapy and cognitive-behavioral therapy can be useful and help with symptoms and mood.
Low FODMAP diet: Working with a doctor or registered dietitian to determine a diet low in FODMAPs is an option for alleviating bloating and distension symptoms. FODMAPs are shortchain carbohydrates that are poorly absorbed in the small intestine and rapidly fermented by bacteria in the gut.
Foods that are rich in FODMAPs include:
- Fruits such as mangoes, apples, pears, avocados, blackberries, and plums
- Dairy products like cow, sheep, and goat milk, as well as yogurt, ice cream, and soft cheeses including cottage cheese, cream cheese and mascarpone
- Honey
- Vegetables and legumes such as asparagus, bell peppers, broccoli, Brussels sprouts, cabbage, cauliflower, eggplant, onion, garlic, baked beans, kidney beans, and lentils
- Sweeteners like sorbitol and maltitol (frequently used in gum and other candies)
Learn more about the low FODMAP diet
Conclusion
Bloating and distension are both very common, for the general population and for those with FGIDs and motility disorders. Either of the two may be very bothersome to individuals that are experiencing the symptoms, as well as challenging to those trying to treat them. There is not a conclusive cause for bloating or distension, nor is there a universally effective treatment. With the help of a physician, individuals can find different treatment options that may help alleviate their symptoms.
For specific guidance regarding personal health questions, we advise consultation with a qualified healthcare professional familiar with your particular circumstances. Be sure to thoroughly discuss treatment options and the use of any medications for treatment with your physician. When prescribed a medication, disclose the use of all other drugs or supplements (whether prescription or over-the-counter) with your physician.
Adapted from IFFGD publication #262 by Max Schmulson, MD, Professor of Medicine, National Autonomous University of Mexico-UNAM, Mexico City, Mexico, Published in Digestive Health Matters Vol. 22 No. 1













