What is an anal fistula?
A fistula is an abnormal connection or tunnel between two organs or two tissue surfaces. An anal fistula is known medically as “fistula-in-ano” and is sometimes also referred to as perianal fistula. Perianal refers to the area of the body surrounding the anus, and particularly the skin in that area. Perianal fistulas are when these abnormal connections or tunnels occur between the anal canal (or rectum) and an external opening in the skin near the anus.
Anatomy
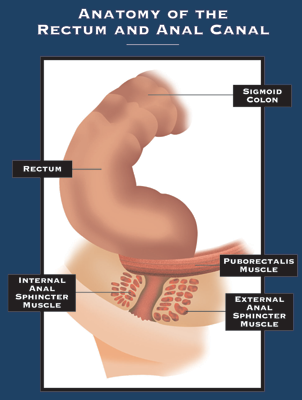
In order to understand the cause, treatment, and complications of therapy for anal fistulas, an understanding of the anatomy of the anal canal (or rectum) is necessary. The anal canal is the terminal (end) portion of the gastrointestinal tract. Two rings of muscle, the internal anal sphincter and external anal sphincter, surround the anal canal. The internal anal sphincter is composed of smooth muscle and is not under voluntary control. The external anal sphincter is composed of skeletal muscle and is under voluntary control. Together these two muscles are very important in the maintenance of the ability to control bowel movements.
Approximately one to two centimeters inside the anal canal, the lining changes. There is a line that marks this change called the dentate line. There are also anal glands located between the layers of the internal and external anal sphincters. These glands contain fluid that will empty into the anal canal at the level of the dentate line. It is when these anal glands get infected that abscesses and anal fistulas can occur. An abscess is a pocket of pus from an infection.
Causes and Symptoms
Perianal fistulas can occur in anyone; however, it is twice as common in men and people assigned male at birth (AMAB). Perianal fistulas are often a result of a specific cause or disease. These can include:
- Colitis
- Crohn’s disease
- Chronic diarrhea
- Diverticulitis
- Chronic sexually transmitted infection (STI)
- Infection with tuberculosis or HIV
- Radiation treatment in the perianal region (such as for rectal cancer)
- Complications of surgery near the anus
- Being immunocompromised (having a weakened immune system) or prone to more frequent infections
People with Crohn’s disease may experience fistulas forming in different parts of the intestines, with another organ, such as the bladder, or through to the skin surface. However, perianal fistulas are the most common type of fistula in Crohn’s disease and can be referred to as perianal Crohn’s fistulizing disease. Research has shown that between 23%-38% of those with Crohn’s disease may develop perianal Crohn’s fistulizing disease.
Anal fistulas and abscesses
Anal fistulas and abscesses of the perianal region are different signs of the same clinical disease. They usually develop in the upper part of the anus, where the anal glands are located. When these glands become infected, they can cause a perianal abscess. The abscesses may break through the skin and drain, causing a fistula. As many as 50% of people with an abscess get a fistula. However, a fistula can also occur without an abscess if there is an injury to the anal canal. This sometimes can happen during surgery to the rectum or anus.
What does an anal fistula look like?
An anal fistula looks like a hole in the skin near your anus. This hole is the portion of the tunnel on the skin which drains the abscess and connects to it inside the body. It might have drainage coming from it, especially when you touch around it. The drainage can be pus, blood and/or bowel movement. Some older fistulas may close at the opening, while the rest of the tunnel remains. This can cause pain and swelling in the area until the fistula reopens to let out the drainage. You may or may not be able to see the fistula with a mirror.
Symptoms
Symptoms of an anal fistula include:
- skin irritation around the anus
- a throbbing pain that may worsen with movement, a bowel movement, or coughing
- smelly discharge near the anus
- passing pus or blood with a bowel movement
- swelling and redness around the anus
- difficulty controlling bowel movements
- fever
Treatment
The goals of treatment for a perianal fistula are the complete closure of the fistula, the elimination of sepsis (if present), the prevention of recurrence, and continence (continued ability to control bowel movements). Combined medical and surgical treatments are used to treat perianal fistulas.
Having a multidisciplinary team which includes a gastroenterologist, radiologist, and colorectal surgeon is important. The treatment and management of perianal fistulas requires precise diagnostics to understand the disease, the correct choice of treatment option, either pharmacological or surgical, or both, as well as a monitoring plan to ensure they do not recur. There are many options and open and honest discussions between the healthcare team and the patient are extremely important.
Summary
Fistulas recur in less than 10% of patients after surgery. In a study from the University of Minnesota, nearly half of the patients treated for fistula-in-ano had some degree of impairment of continence after treatment. Most of these individuals had problems with staining their underclothes or holding gas, but a minority of patients had accidental bowel movements.
Fistula-in-ano is a common condition that usually follows infection of an anal gland. Treatment is directed at eliminating infection, while preventing recurrence and incontinence after surgery.
Most patients are readily treated by simply laying open the fistula tract. However, minor changes in continence do occur in a significant number of patients. Other available options include the use of setons or advancement flaps.
CoRDS Anal Fistulas Questionnaire
IFFGD has created an anal fistula questionnaire with CoRDS. To access this questionnaire, please click here.
About Coordination of Rare Diseases at Stanford (CoRDS)
Based at Sanford Research, a nonprofit research institution, CoRDS is a centralized international patient registry for all rare diseases. They coordinate the advancement of research into 7,000 rare diseases.
Adapted from “Anal Fistulas”- IFFGD Publication #138 by Satish Rao, MD, Harold Harrison, MD,
Distinguished University Chair in Gastroenterology, Department of Gastroenterology/Hepatology, Augusta University, Augusta, Georgia














